The new investigation focused on the failure of a procedure known as “mismatch fix.”
A Yale University study offers a new clarification for why immunotherapy only performs for some most cancers individuals.
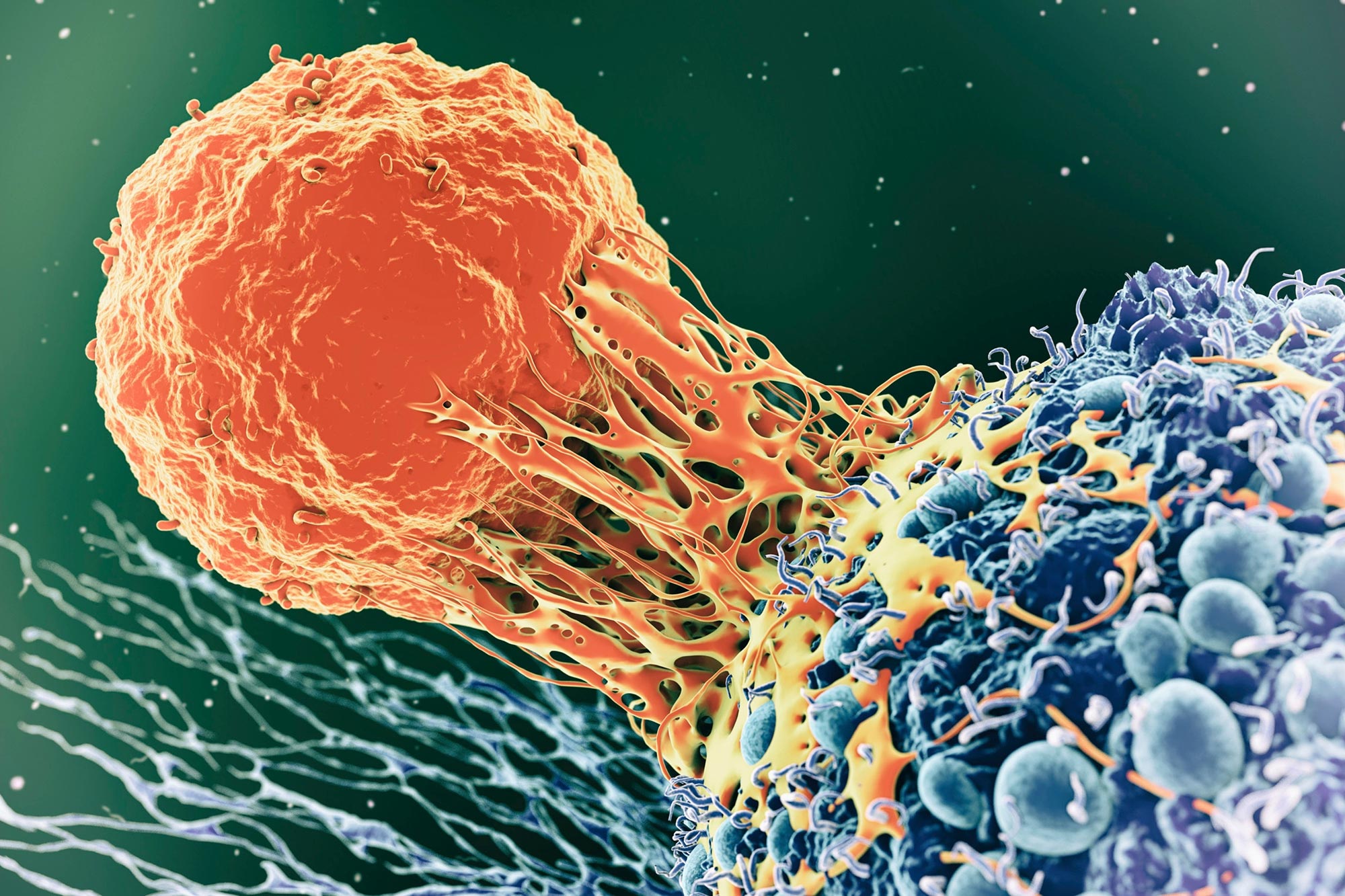
Immunotherapy, a biotherapy that enhances the immune system’s capability to realize and struggle mutant tumor cells, has transformed the therapy landscape for sufferers struggling from cancer, which is brought on by the progressive accumulation of
“We wanted to understand why some patients respond better than others to immunotherapy,” said co-corresponding author Ryan Chow, an M.D./Ph.D. candidate working in Yale’s Department of Genetics and the Systems Biology Institute.
The Yale team’s research concentrated on the failure of a process known as “mismatch repair.” When cells divide, errors in their DNA often arise. A special group of proteins identifies and corrects DNA errors through mismatch repair. However, a breakdown in this editing process occurs in many different types of cancer, resulting in high mutation levels.
The research team — led by Chow, Dr. Eric Song, an ophthalmology resident and former M.D./Ph.D. student at Yale, and Dr. Alessandro Santin, a professor of obstetrics, gynecology, and reproductive sciences — zeroed in on the fact that mismatch repair deficiency can result from two distinct mechanisms. In one, mutations occur in the DNA repair machinery itself, leading to the production of defective repair proteins; in the second, production of the DNA repair machinery is halted entirely. In both cases, the tumors accumulate very high levels of mutations that would be expected to make them good candidates for immunotherapy.
“An analogy would be a dysfunctional toy factory,” Chow said. “Maybe the factory makes broken toys that don’t work, or the factory has no personnel and stops producing toys altogether. Either way, kids won’t be happy.”
However, the researchers found that tumors with defective DNA repair proteins had significantly better responses to immunotherapy than those in which the production of DNA repair proteins had been silenced. These differences could ultimately be traced to changes in the immune response that was mounted against each of the two classes of tumors, they said.
“When it comes to immunotherapy, it seems that the journey — in this case, the underlying cause of mismatch repair deficiency — may be just as important as the destination,” Chow said.
Added Song: “The innovative use of clinical trial data can guide our understanding of how immunotherapy manipulates the immune system and ultimately improve how we treat patients.”
Reference: “Distinct mechanisms of mismatch repair deficiency delineate two modes of response to PD-1 immunotherapy in endometrial carcinoma” by Ryan D. Chow, Tai Michaels, Stefania Bellone, Tobias MP. Hartwich, Elena Bonazzoli, Akiko Iwasaki, Eric Song and Alessandro D. Santin, 27 October 2022, Cancer Discovery.
DOI: 10.1158/2159-8290.CD-22-0686
Santin is part of the Yale Cancer Center and Song is a resident at Smilow Cancer Hospital.






