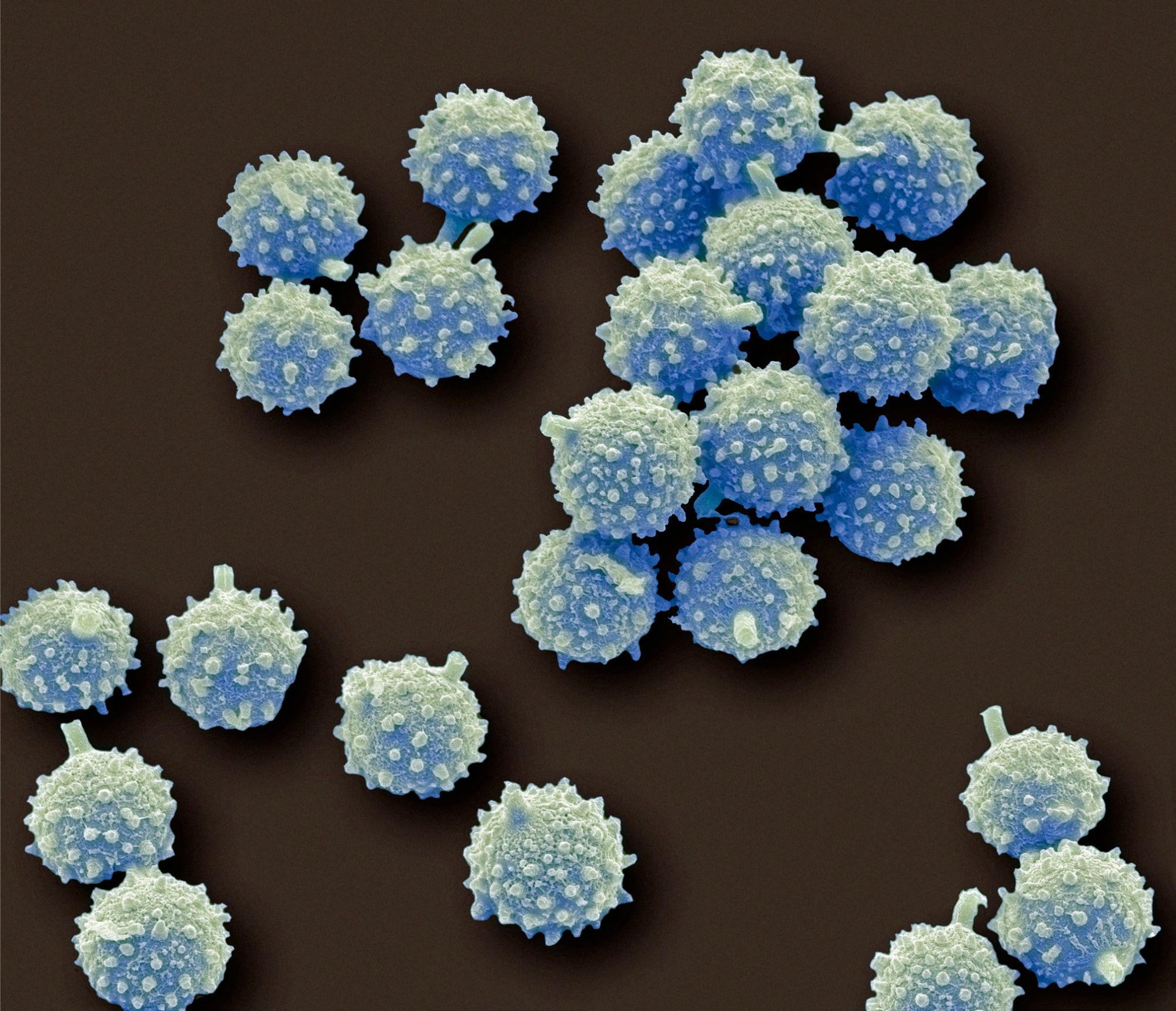
Aspergillus is a form of fungus usually observed in soil and decaying organic and natural make a difference. Although some species of Aspergillus are benign, many others can lead to bacterial infections in folks with weakened immune methods, foremost to conditions this sort of as aspergillosis.
The discovery reveals a new focus on for combating the fatal invader.
Aspergillus and other fungi are so ubiquitous in our natural environment that we inhale hundreds to thousands of spores every day. Normally, they do not pose a hazard to healthful individuals, but can verify lethal to all those with weakened immune methods. Even so, it is getting to be more and more comprehended that viral infections like influenza or
“We discovered that influenza and COVID-19 destroy a previously unknown natural immunity that we need to resist invasive fungal infections,” says Nicole Sarden, a Ph.D. candidate at the University of Calgary and first author on the study.
The findings published in Science Translational Medicine show that two types of white blood cells (neutrophils and a unique type of B cells) normally work together to fight fungal infection. However, viruses like SARS-CoV-2 and influenza impede the special B cells from doing their job. Working with mice and human blood and tissue samples, the researchers were able to see that following a viral infection, neutrophils sensed a fungal infection and were gathering nearby, but weren’t acting to destroy the invader as expected. The scientists delved further and learned that viral molecules were rendering these B cells apathetic, preventing them from cooperating with neutrophils as they normally would, and thus protecting the fungi from destruction. Understanding this process led to the next discovery.
“We also found that current therapies exist that could be repurposed in a realistic and meaningful way to replace the natural antibodies not being produced by the virally-damaged B cells and re-establish the neutrophils’ ability to fight these infections,” says Sarden.
“This research was sparked by a young man I cared for in the ICU on life support who died of influenza-associated aspergillosis, where every therapy we tried failed,” says Dr. Bryan Yipp, MD, clinician-researcher at the Cumming School of Medicine and senior author on the study. “Our findings are very timely given the high numbers of patients affected by multiple respiratory viruses including influenza.”
Sarden and Yipp believe these findings will lay the groundwork for new diagnostic tests, based on natural antibody levels to predict who is at the highest risk for invasive fungal infections, and that currently available antibody replacement strategies could be tested to treat Aspergillus infections in future clinical trials.
“These discoveries provide a new understanding of how we can best support the body to fight off deadly fungal infections,” says Yipp.
Reference: “A B1a–natural IgG–neutrophil axis is impaired in viral- and steroid-associated aspergillosis” by Nicole Sarden, Sarthak Sinha, Kyle G. Potts, Erwan Pernet, Carlos H. Hiroki, Mortaza F. Hassanabad, Angela P. Nguyen, Yuefei Lou, Raquel Farias, Brent W. Winston, Amy Bromley, Brendan D. Snarr, Amanda Z. Zucoloto, Graciela Andonegui, Daniel A. Muruve, Braedon McDonald, Donald C. Sheppard, Douglas J. Mahoney, Maziar Divangahi, Nicole Rosin, Jeff Biernaskie and Bryan G. Yipp, 7 December 2022, Science Translational Medicine.
DOI: 10.1126/scitranslmed.abq6682
The study was funded by the Canadian Institutes of Health Research.






