Osteoarthritis is a degenerative joint disease that causes the cartilage in the joints to crack down, main to soreness, stiffness, and issue shifting. It is a popular problem that normally impacts the arms, knees, hips, and spine. Threat things for acquiring osteoarthritis consist of getting old, weight problems, and a history of joint accidents.
Two the latest scientific studies have demonstrated that corticosteroid injections, which are typically made use of to take care of the soreness related with knee osteoarthritis, may possibly actually add to the development of the illness. These findings have been lately presented at the once-a-year meeting of the Radiological Society of North The us (RSNA).
Osteoarthritis is a prevalent situation that impacts 32.5 million grownups in the United States and is characterised by the degeneration and breakdown of cartilage in the joints. Knee osteoarthritis, which affects around 800,000 people each 12 months, is a chronic and progressive affliction that can bring about soreness and issue transferring. Somewhere around 10{2c3a8711102f73ee058d83c6a8025dc7f37722aad075054eaafcf582b93871a0} of persons with knee osteoarthritis find noninvasive solutions and switch to corticosteroid or hyaluronic
Researchers in both studies chose cohorts from the Osteoarthritis Initiative, a multicenter, longitudinal, observational study of nearly 5,000 participants with knee osteoarthritis currently in its 14th year of follow-up.

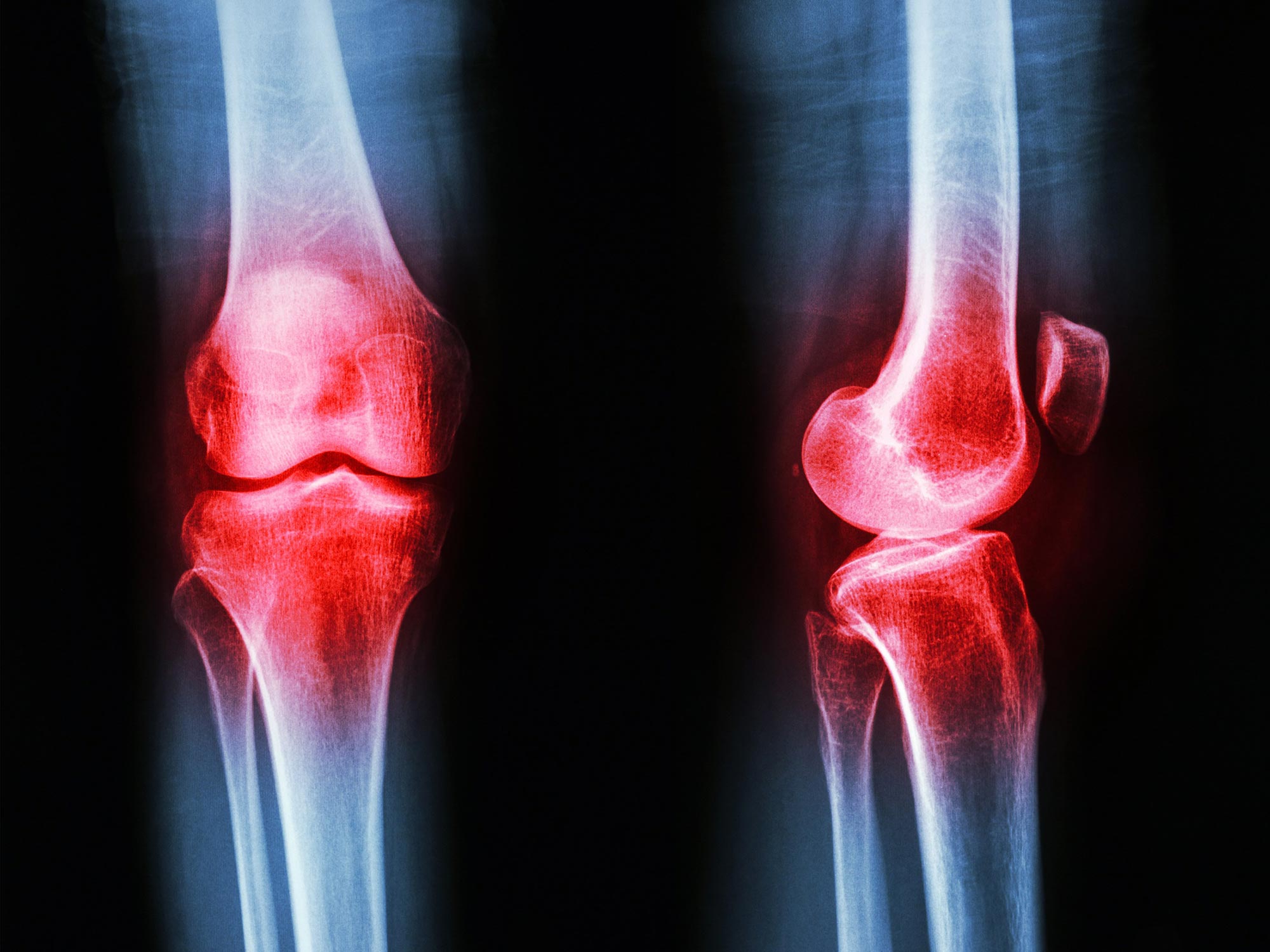
Knee joint of a patient showing (A) severe cartilage defects and (B) intact knee joint. Credit: RSNA and Upasana Upadhyay Bharadwaj, M.D.
In the first study, researchers at the University of California, San Francisco included 210 Osteoarthritis Initiative participants, 70 of whom received intraarticular injections, and a control group of 140 who did not receive injections during a two-year period. Of the 70 patients who received injections, 44 were injected with corticosteroids, and 26 were injected with hyaluronic acid. The treatment and control groups were matched by age, sex, body mass index, pain and physical activity scores, and severity of the disease.
MRI was performed on all patients at the time of the injection and two years before and after. The MRI scans were assessed using whole-organ magnetic resonance imaging score (WORMS), a grading system for knee osteoarthritis that focuses on the meniscus, bone marrow lesions, cartilage, joint effusion, and ligaments. The researchers identified osteoarthritis progression by comparing the imaging scores from the initial scans and two-year follow-up scans.
“This is the first direct comparison of corticosteroid and hyaluronic acid injections using the semi-quantitative, whole organ assessment of the knee with MRI,” said Upasana Upadhyay Bharadwaj, M.D., a research fellow in the Department of Radiology at University of California, San Francisco.
Statistical analysis showed that corticosteroid knee injections were significantly associated with the overall progression of osteoarthritis in the knee, specifically in the lateral meniscus, lateral cartilage, and medial cartilage.
Hyaluronic acid knee injections were not significantly associated with the progression of osteoarthritis in the knee. Compared to the control group, the group who received hyaluronic injections showed a decreased progression of osteoarthritis, specifically in bone marrow lesions.
“While both corticosteroid and hyaluronic acid injections are reported to help with symptomatic pain relief for knee osteoarthritis, our results conclusively show that corticosteroids are associated with significant progression of knee osteoarthritis up to two years post-injection and must be administered with caution,” Dr. Upadhyay Bharadwaj said.
“Hyaluronic acid, on the other hand, may slow down the progression of knee osteoarthritis and alleviate long-term effects while offering symptomatic relief.”
In the second study, researchers at the Chicago Medical School of Rosalind Franklin University of Medicine and Science conducted a case-control study comparing the radiographic progression of osteoarthritis in patients who received injections of corticosteroids and hyaluronic acid.
“While these injections provide some patients with short-term pain relief, the effects of the injections on the progression of the disease are unknown,” said researcher and medical student Azad Darbandi.
Darbandi’s team selected a cohort of 150 patients with similar baseline characteristics from the Osteoarthritis Initiative database, including 50 patients who received corticosteroid injections, 50 who received hyaluronic acid injections, and 50 who were not injected over a 36-month time period. The groups were matched by sex, body mass index, and X-ray findings.
Patients underwent X-ray imaging of the knee at baseline and two years later. The researchers analyzed the X-ray imaging, including joint space narrowing, formation of bone spurs, and bone thickening around the knee cartilage.
Compared to patients who received an injection of hyaluronic acid or no treatment at all, patients injected with corticosteroids had significantly more osteoarthritis progression, including medial joint space narrowing, a hallmark of the disease.
“Even though imaging findings for all patients were similar at baseline, the imaging hallmarks of osteoarthritis were worse two years later in patients who received corticosteroid injections compared to patients who received hyaluronic acid injections or no treatment at all,” Darbandi said.
“The results suggest that hyaluronic acid injections should be further explored for the management of knee osteoarthritis symptoms and that steroid injections should be utilized with more caution.”
“Knowing the long-term effects of these injections will help osteoarthritis patients and clinicians make more informed decisions for managing the disease and the pain it causes,” Dr. Upadhyay Bharadwaj added.
Meeting: 108th Scientific Assembly and Annual Meeting of the Radiological Society of North America
Dr. Upadhyay Bharadwaj’s co-authors are Thomas Link, M.D., Ph.D., Zehra Akkaya, Gabby Joseph, John Lynch, Ph.D., and Paula Giesler. Darbandi’s co-authors are Sean Hormozian, Atefe Pooyan, M.D., Ehsan Alipour, M.D., Firoozeh Shomal Zadeh, M.D., Parham Pezeshk, M.D., and Majid Chalian, M.D.






